CONNECT IN THE MORNING
Fits into your day
No more setting an alarm to remind you to take your levodopa pills every few hours! Just connect the Duopa pump in the morning to get levodopa delivered continuously over 16 hours throughout the day.
BYPASSING THE STOMACH DELIVERS LEVODOPA WHERE YOU NEED IT
Duopa is delivered right into the intestine, so your levodopa can be absorbed quickly.
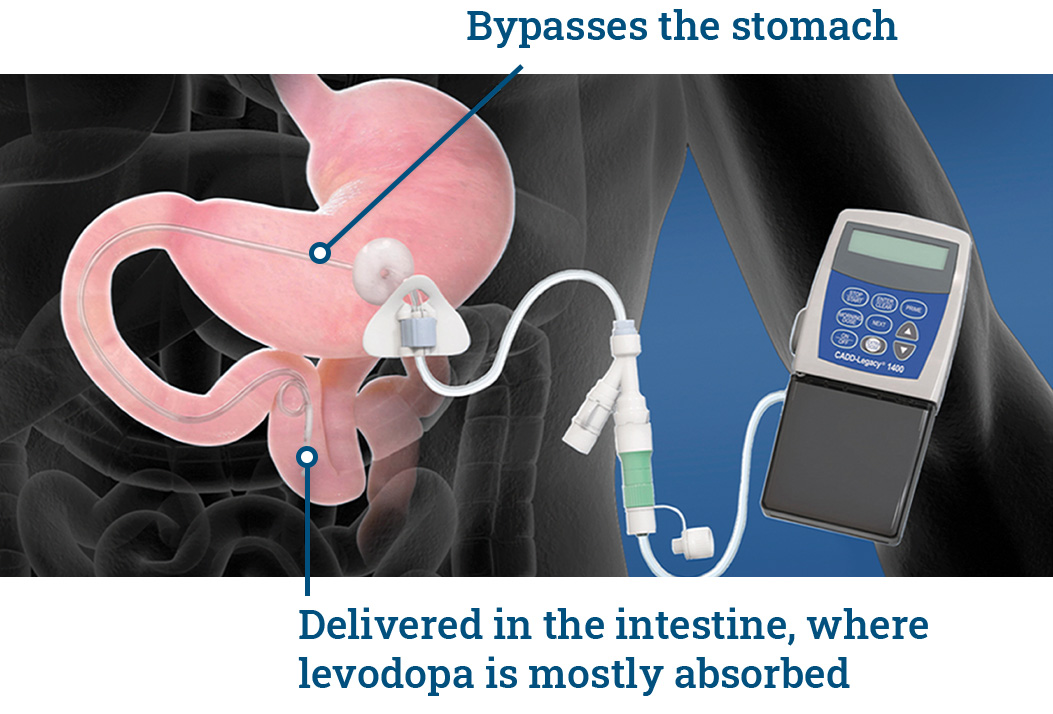
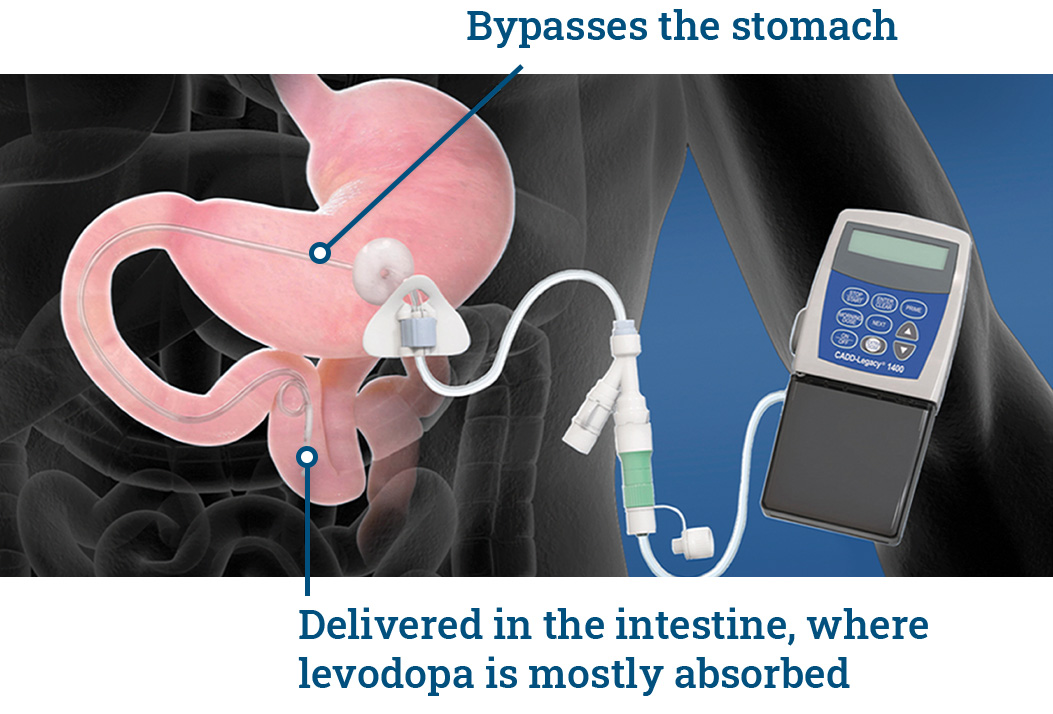
To prepare you for Duopa, a specialist makes a small hole (called a “stoma”) in the stomach wall and places a medication delivery port.* Afterward, your doctor connects a portable pump to deliver levodopa continuously over 16 hours.
*A percutaneous endoscopic gastrostomy with jejunal tube (or “PEG-J”).
Selected Important Safety Information
Your healthcare provider will talk to you about the stoma procedure. Before the stoma procedure, tell your healthcare provider if you ever had a surgery or problems with your stomach.
Talk to your healthcare provider about what you need to do to care for your stoma. After the procedure, you and your healthcare provider will need to regularly check the stoma for any signs of infection. Symptoms of infection may include: drainage, redness, swelling, pain, or feeling of warmth around the small hole in your stomach wall (stoma).
YOUR DAILY ROUTINE
Because levodopa is delivered continuously over 16 hours, you won’t need to take your levodopa pills so often. Just connect the Duopa pump in the morning to get levodopa delivered continuously throughout the day.
You’ll take a Duopa cassette out of the refrigerator and let it sit for 20 minutes at room temperature. Connect the pump to the cassette and then the stomach tube. Start the pump to get a morning dose. Your continuous dose will start automatically.
CONTINUOUS LEVODOPA DELIVERY OVER 16 HOURS
DISCONNECT AT NIGHT
After 16 hours, you’ll disconnect the pump. Flush the stomach tube with drinking water and discard the Duopa cassette. You can take a nighttime dose of oral carbidopa/levodopa pills if prescribed by your doctor.
Your doctor will decide if you need extra medicine during the day. If you feel that your medicine is wearing off, you can give yourself an extra dose through the pump. (Keep in mind that frequent extra doses may cause or worsen dyskinesia.)
Selected Important Safety Information
Do not stop using DUOPA or change your dose unless you are told to do so by your healthcare provider. Tell your healthcare provider if you develop withdrawal symptoms such as fever, confusion, or severe muscle stiffness.
YOU AND YOUR DOCTOR ARE IN CHARGE SINCE THE PROCEDURE IS REVERSIBLE
If you need to discontinue treatment or you and your doctor ever change your mind about Duopa, the procedure can be reversed. This lets you keep your options open for the future.
The medication delivery port can be completely removed by a specialist so the stoma heals. Do not stop using Duopa or change your dose unless you are told to do so by your doctor. Tell your doctor if you develop withdrawal symptoms, such as fever, confusion, or severe muscle stiffness.
Selected Important Safety Information
Talk to your healthcare provider about what you need to do to care for your stoma. After the procedure, you and your healthcare provider will need to regularly check the stoma for any signs of infection. Symptoms of infection may include: drainage, redness, swelling, pain, or feeling of warmth around the small hole in your stomach wall (stoma).
WHAT DO REAL DUOPA PATIENTS THINK?
To connect with a Peer Mentor, call 1-855-776-8966 or enroll here.
